Vitamin D3 Derivates: Calcipotriol Tacalcitol Calcitriol
Vitamin D analogs regulate epidermal cell proliferation and differentiation, as well as production and release of proinflammatory cytokines. Topical formulations containing vitamin D3 and vitamin D analogs are effective treatments for PP, both as monotherapies and in fixed combinations with corticosteroids. Vitamin D3 derivates appear to be more effective in treating nail bed signs of psoriasis than in nail matrix signs. Studies using calcitriol in the treatment of nail psoriasis are rare. One case was reported whereby the patient responded well to treatment with calcitriol ointment however, it was not completely clear whether this patient suffered from nail psoriasis. One RCT compared calcitriol ointment twice daily with betamethasone diproprionate on subungual hyperkeratosis . After 20 weeks, nails treated with calcitriol had a 38 % reduction in thickness compared with a 35 % reduction seen in nails treated with betamethasone diproprionate .
Or Maybe Athletes Foot Has Taken Your Little Piggies Hostage
Athletes foot occurs when a fungal infection affects the skin on your feet.
Signs of athletes foot include:
- dry skin on the soles and sides of the feet
- burning and itching between the toes or on the soles
- cracking, peeling skin on the feet
Toenail fungus infections can often arise from athletes foot.
Treatment Options And Lifestyle Changes
There are several things you can do that can provide relief from skin and nail psoriasis and psoriatic arthritis .
Once nail psoriasis is suspected, the sooner you start treatment, the better. Coordination of care between a dermatologist and a rheumatologist can provide a patient with the best course of treatment.
Siegel says several systemic and biologic treatments that work for psoriasis and PsA can also work for nail psoriasis. Talk to your health care team to find out if this approach might be effective for you.
Topical corticosteroids can be applied to the nail matrix with the goal of absorbing into the still-forming nail. Patients also have the option of having corticosteroids injected into the affected nail. However, the pain of the procedure can be a deterrent to this treatment.
Using nail polish and nail polish remover with harsh chemicals such as parabens, formaldehyde and acetone can dry out the nails and cause further brittleness and possibly pain.
Siegel and Prussick agree that being overweight can contribute to a person with psoriasis developing PsA. When belly fat increases, the amount of harmful inflammatory cytokines in the body also increases. In addition, there is some speculation that repeated stress on the joints can add to the development of PsA.
Going for a 30-minute walk every day, staying away from high glycemic foods and managing stress can help keep psoriasis and PsA symptoms from worsening.
Recommended Reading: How Long Does Liquid Nails Take To Dry
When Should You See A Doctor
See a doctor if you notice discoloration, pitting, or cracking in your nails. If you have psoriasis or diabetes, this is extremely crucial because, as per research, theres a good chance that you could be suffering from both conditions.
Are you suffering from nail psoriasis or nail fungus? Schedule an appointment with MI Express Care. Our doctors can develop a recovery plan to diagnose and treat nail psoriasis and nail fungus accurately.
Tags:
Pathogens In Psoriatic Nails
Numerous studies in the literature have reported the various fungal pathogens that may cause onychomycosis in patients with nail psoriasis and have demonstrated the percentages for the responsible fungi . However, evidence has been contradictory and the reason for these rather different results is still not completely understood.
Read Also: Is Toenail Fungus Covered By Medicare
Treatment Options For Nail Psoriasis Toenail Psoriasis And Nail Fungus
Since the causes of nail psoriasis and nail fungus differ, the treatments for both are also different. Antifungals, either topically or orally, are used to treat nail fungus because it is an infection. Since psoriasis is an inflammatory condition, treatment involves assessing the triggers and reducing inflammation. You will may also be prescribed a steroid.
What Are The Differences
There are a few key differences between the two conditions. Nail fungus has a few symptoms that generally dont occur in nail psoriasis. These include:
- Debris under the nail that can look dark in color2,4
- Brittle nails that are more likely to split2,4
- A mild, foul-smelling odor2
Nail psoriasis also has a few unique symptoms, that dont usually occur in fungal infections. These include:
- Pitting of the nail, 1
- Deformed nail shape3
Read Also: What Is The Best Uv Led Nail Lamp
When To See A Doctor
If you suspect psoriasis or have a family history of psoriasis, reach out to your healthcare provider. If you have a new, worsening dark discoloration on one nail in particular, though rarer, this can be a sign of melanoma of the nail.
If you suspect mild fungus, you may manage the symptoms with over-the-counter creams. If creams dont improve symptoms in a few weeks, visit your healthcare provider. Nail fungus usually requires an oral prescription antifungal for successful treatment.
Good hygiene cant prevent psoriasis, but it can help ward off fungal infections.
Fight the fungus with these tips:
- Keep your nails trimmed and clean to prevent fungal growth.
- Avoid cleaning under your nails with sharp tools.
- Use nail moisturizers and oils to keep your nails healthy and soft.
- Avoid tight shoes that cram toes together.
- Dont go barefoot in public .
- Keep your feet and hands dry.
- Wear clean, breathable socks.
Whats The Difference: Nail Psoriasis Vs Fungus
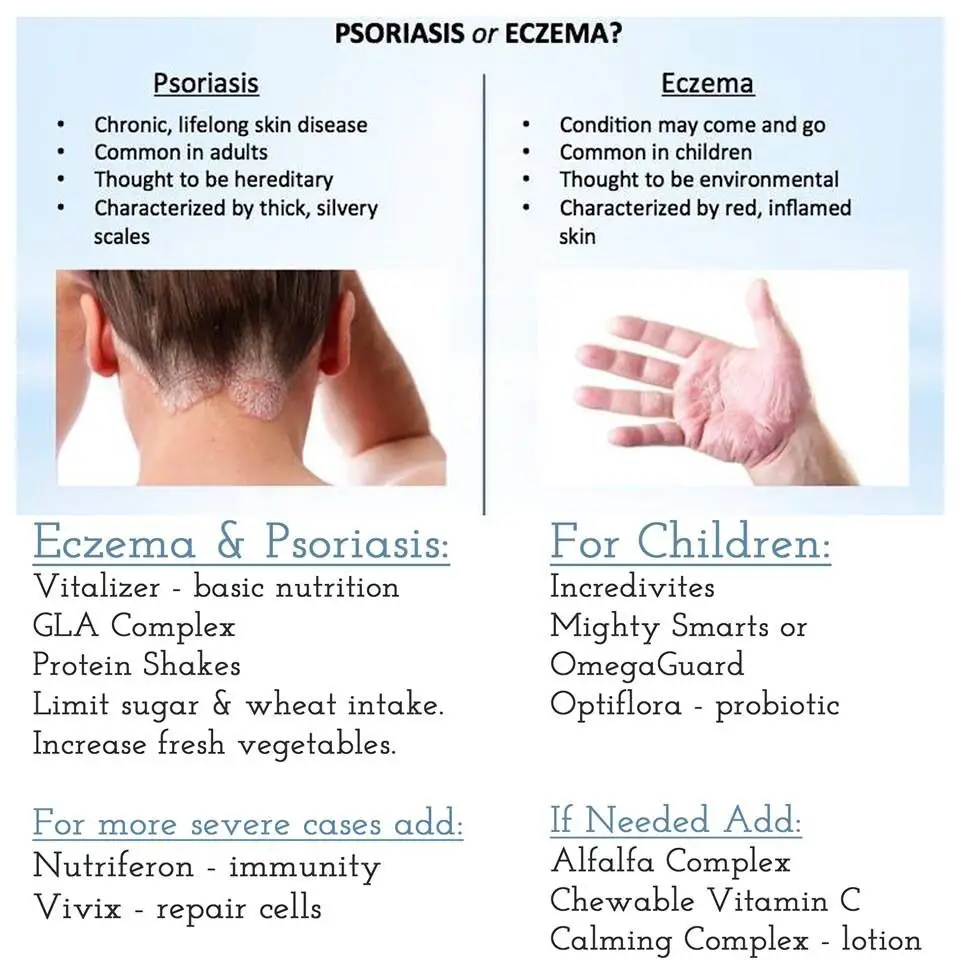
Did you know that psoriasis can also affect your nails? As an autoimmune disease that causes the rapid overgrowth of skin cells, nail psoriasis can resemble nail fungus. This makes it difficult for people to tell them apart and get proper treatment.
Understanding the difference between nail psoriasis vs. fungus is highly important. It can help symptoms from worsening or infection from spreading. Read on to learn how to tell nail psoriasis vs. fungus apart.
Recommended Reading: Is Collagen Good For Your Nails
What Is Nail Psoriasis And Who Does It Affect
Nail psoriasis or psoriatic nail dystrophy is a form of psoriasis that affects the nails. Psoriasis is a chronic, immune-mediated skin condition that causes skin-cell growth to speed up and the cells to pile up on the surface of the skin. It affects about 2-3 percent of people worldwide.Nail psoriasis is not infectious and typically occurs in about 50 percent of people who have psoriasis elsewhere on their body, often developing some years after psoriasis has appeared on the skin. Although, in some cases nail psoriasis can occur in people with no other signs of psoriasis. Nail psoriasis is a risk factor for psoriatic arthritis.
Prevention Of Nail Psoriasis
Good nail care is the best way to treat nail psoriasis. Try these prevention tips:
- Keep your nails trimmed short.
- Use a nail file to keep nail edges smooth.
- Wear gloves to clean and do other work with your hands.
- Moisturize your nails and cuticles every day and after theyve been in contact with water.
- Wear comfortable shoes with enough room for your toes.
If youre unhappy with the way your nails look, try nail varnish or artificial nails. They can also protect your nails from more damage. Some people are sensitive to the chemicals in varnish and nail adhesive. Talk to your doctor about whether these are right for you.
Dont Miss: How To Apply Liquid Nails
Recommended Reading: Can Hiv Transmitted Through Nail Scratch
Psoriasis Or Nail Fungal Infection How To Tell
7.5k Views
Although it is a relatively common disease, when it comes to nail fungal infections, theres a possibility of getting a false diagnosis, one that confuses onychomycosis with nail psoriasis, two completely different pathologies.
Therefore, performing a laboratory test is essential to determine if theres a microorganism causing an infection or not.
How can you differentiate them at plain sight? Keep reading!
Let’s Take A Look At Risk Factors
As discussed earlier, having psoriasis can put you at risk for nail fungal infections. While the only risk for getting nail psoriasis is having psoriasis on your hands and feet, there are quite a few risk factors for nail fungus.2,4
- Age: You are more likely to get nail fungus infections as you get older. This can because your nails grow slower, your circulation is not as good, and because you have been exposed to more fungi than when you were younger.
- Having other health issues: Patients with cancer, diabetes, poor circulation, and poor immune systems are more likely to have nail fungal infections.
- Exposure to damp environments: Fungus thrives in damp environments. If you notice that your socks are damp every time you take them off, you have to wear gloves a lot for your job, or you often walk barefoot in places like locker rooms, or pools, you are at higher risk for nail fungal infections.
- Wearing artificial nails: Make sure that your salon uses new or freshly sterilized instruments every time you get your nails done. Additionally, acrylic nails can separate from the natural nail, leaving a place for fungus to grow.
Read Also: How Do I Remove Acrylic Nails
Risk Factors For Nail Psoriasis And Nail Fungus
Fungi are microscopic organisms that thrive in damp, warm settings. Showers and swimming pools are two of their favorite locations to hide. Any gap between your nail and the nail bed is an invitation for fungus to invade. They can even get in through small cuts in your skin. With age, you’re more likely to develop nail fungus. Men are more likely than women to get nail fungus, especially if they have a family history of fungal diseases. Additionally, according to the National Psoriasis Foundation, about 50% of people with psoriasis and over 80% of people with psoriatic arthritis have nail-related medical issues. You’re also more likely to get nail fungus if you
- Sweat profusely
- Work in a humid setting where your hands or feet are frequently wet
- Walk barefoot around public pools, gyms, and showers
- Wear socks and shoes with insufficient ventilation
- Live with a person suffering from nail fungus
- Have an immunosuppressive health condition such as HIV
People with circulatory issues or diabetes are also more vulnerable. Any injury to the nail bed can increase your risk of developing nail fungus. With nail psoriasis, it’s unclear why some people with psoriasis have problems with their nails while others dont.
Treatment Options For Nail Fungus
When it comes to nail fungus, the first treatment option is an over-the-counter antifungal medication. In the cases that these do not work, your podiatrist may recommend:
- Getting a culture to determine the cause of the fungus.
- Using prescription-strength topical or oral antifungals.
- Removing the diseased nail.
Don’t Miss: Does Hongo Killer Nail Formula Work
Diagnosing: Another Method Of Determining
It so happens that psoriasis can be accompanied by a fungal infection due to disruptions in immunity, metabolism, and other changes. In those cases, additional diagnostic methods might be needed.
Microscopic examination of a piece of the affected nail is needed to determine the pathogenic fungal flora that accompanies psoriasis.
Steroid Injections And Creams
People who suffer from certain autoimmune diseases, such as rheumatoid arthritis and psoriasis, may receive steroid injections. Steroids give the immune system a boost, which makes them effective at easing symptoms of certain autoimmune diseases.
With nail psoriasis, steroids are injected into the nail bed.
Steroid creams are another option that may be more effective for milder cases of nail psoriasis.
Also Check: How Do You Remove Impress Nails
For Best Results From Treatment
Treating nail psoriasis can be a challenge. It often takes time to treat. To get results, you need to treat your nails as directed and for as long as directed. Some patients need to try a few treatments to find one that works.
The right nail care can help you get the best results from treatment. Youll find out what dermatologists recommend at: 7 easy-to-follow nail care tips that can reduce nail psoriasis
ImagesImages used with permission of the Journal of the American Academy of Dermatology. J Am Acad Dermatol 2013 69:249.
ReferencesCrowley JJ, Weinberg JM, et al. Treatment of nail psoriasis: Best practice recommendations from the Medical Board of the National Psoriasis Foundation. JAMA Dermatol. 2015 Jan 151:87-94.Dogra A, Arora AK. Nail psoriasis: The journey so far. Indian J Dermatol. 2014 Jul 59:319-33.Lin YK, Chang YC, et al. A Chinese herb, indigo naturalis, extracted in oil used topically to treat psoriatic nails: A randomized clinical trial. JAMA Dermatol. 2015 Jun 151:672-4.Manhart R, Rich P. Nail psoriasis. Clin Exp Rheumatol. 2015 Sep-Oct 33:7-13.van der Velden HMJ, Klaassen KMG, et al. Fingernail psoriasis reconsidered: A case-control study. J Am Acad Dermatol 2013 Aug 69:245-52.
All content solely developed by the American Academy of Dermatology
The American Academy of Dermatology gratefully acknowledges the support from Bristol Myers Squibb.
What Is A Nail Fungal Infection And Who Does It Affect
Onychomycosis is a chronic infection of a toenail or fingernail caused by a fungus. Usually nail fungal infections are caused by dermatophytes, but molds and yeasts can also infect nails. A nail fungal infection caused by dermatophyte is called tinea unguium, while onychomycosis is a broader term which is now used to describe both dermatophyte and non-dermatophyte nail infections.
Nail fungal infections are more common than nail psoriasis, with cases occurring in about 10 percent of the general population. They are also more common in older people – occurring in 20 percent of people over 60 years of age and 50 percent of people over 70 years age.
Nail fungal infections are more common in older adults because as we age our nails become more dry and brittle. Poorer circulation and a less effective immune system may also play a role. People are also more at risk of developing a nail fungal infection if they have injured the nail, or have a condition such as diabetes or nail psoriasis.
Fungal infections can be picked up from objects, other people, or spread from other sites on your own body. For example, athletes foot , which is a fungal infection commonly found between the toes, can spread to infect nails.
Recommended Reading: Manicure Table With Built In Led Light
Key Difference: Nail Psoriasis Vs Fungus
Apart from the symptoms mentioned above, the main difference is that fungal infections are contagious and psoriasis is not. This makes telling the conditions apart incredibly important, in order to stop the spread. In addition, youre more likely to get nail fungus if you sweat a lot or walk barefoot around public swimming pools, gyms, and showers.
Nail Infection Needs Treatment Too

A nail infection can develop if you have nail psoriasis. Because a nail infection can look a lot like nail psoriasis, its important to find out if you have an infection. Testing, which usually consists of scraping the nail, can find an infection. If you have a nail infection, treatment can get rid of it.
You May Like: How Many Nails Per Square Of Shingles
Dermatophytes Supported To Be The Most Frequently Involved Fungal Agents
In the study by Zisova et al. among patients who developed onychomycosis of psoriatic nails, dermatophytes were observed in 67% , T. mentagrophytes , T. verrucosum ), yeasts in 24% , Candida non albicans ), NDMs in 6% and mixed infection in 3% of patients . According to the authors, infection of the toenails is frequently due to dermatophytes, whereas yeasts are most common in fingernails.
Kacar et al. showed that the most common type of fungus was dermatophytes in patients with psoriasis and NDMs in a healthy group . Dermatophytes were more common in psoriasis patients than in healthy individuals , whereas the incidence of NDMs was found to be similar between psoriatic and healthy groups. The authors assumed that damage of the keratinocytes due to psoriasis may provide an ideal environment for dermatophytes. T. rubrum has been reported as the most common pathogen among dermatophytes in psoriatic patients. The authors concluded that psoriatic nails are a risk factor not for onychomycosis, but specifically for dermatophyte nail infections, and they claimed that the faster growth of psoriatic nails does not protect against dermatophyte infection.
Yeasts Implicated As Fungal Agents
The incidence of yeast-induced onychomycosis in patients with nail psoriasis is reported to be 19â23% . Several studies have shown that yeasts have a higher probability of developing fungal infection in psoriatic nails. Specifically, in the study published by Rizzo et al. , it was reported that in psoriatic patients with onychomycosis, the most common pathogens were Candida spp. compared with dermatophytes . In contrast, non-psoriatic patients with onychomycosis were more likely to have dermatophyte fungal nail infections. However, the results of this research were not statistically significant .
A 2-year Pakistan study by Tabassum et al. reported that the main fungi pathogen in both psoriatic and non-psoriatic group was Candida as the most common), followed by NDMsâAspergillus spp. , and last by dermatophytes . A similar size study by Larsen et al. found that the prevalence of yeasts in psoriatic patients was higher krusei) than the prevalence of dermatophytes . This study estimated that there was no statistically significant difference between the prevalence of dermatophytes in both cases and controls.
Tsentemeidou et al. found that yeast and molds were the main fungal pathogens isolated by mycological testing. Similar results were reported by Natarajan et al. , who concluded that the percentage of fungal culture in psoriatic patients was the same for both yeasts and NDMs .
Recommended Reading: Manicure Pedicure At Home Services
Miscellaneous Systemic Therapies: Fumaric Acid Esters Sulfasalazine And Leflunomide
Fumaric acid esters , sulfasalazine, and leflunomide have also been reported to be effective in nail psoriasis however, based on the current knowledge, they cannot be advised for this indication. FAEs have been used for the treatment of chronic PP since 1959. The commercially available form, containing mainly dimethylfumarate, is currently a first-line systemic therapy for severe chronic PP in several European countries it is not effective in PsA. The general opinion is that it has little efficacy in nail psoriasis, but one case has been reported in which it was effective both on nail bed and nail matrix psoriasis . Side effects are frequent in patients using FAEs, such as episodes of flushing, abdominal pain, and a decrease in lymphocyte count.
Sulfasalazine is an aminosalicylate used as a traditional disease-modifying antirheumatic drug for the treatment of peripheral involvement in PsA. Sulfasalazine is metabolized by gut flora into sulfapyridine and 5-aminosalicylic acid, which act as anti-inflammatory agents. The role of sulfasalazine in cutaneous psoriatic lesions and nail psoriasis is not generally accepted. One case has been reported on the use of sulfasalazine in the treatment of psoriatic nail lesions . After 3 months, nail lesions started to recede and disappeared progressively. No other cases have been reported in literature.