What Do Psoriatic Arthritis Nails Look Like
There isnt a one-size-fits-all answer to this. If youre living with PsA, you may see a variety of changes in your nails, depending on where the inflammation is. PsA is different for everyone. In the initial stages, you may notice only fatigue and joint pain, and your doctor might not yet diagnose PsA.
As PsA progresses, you may start to notice nail changes and swollen toes or fingers. Because its essential to start treatment as soon as possible, you should look out for the following nail changes:
The Correlation Between Different Manifestations Of Psoriasis
Psoriatic arthritis develops in 726% of those with psoriasis vulgaris . The presence of skin lesions precedes articular symptoms typical of PsA in 7580% of patients with a mean estimated delay of 10 years . However, nail changes are observed in 40% of psoriasis patients and up to 80% of those with PsA . This fact became the basis for numerous studies exploring the relationship of nail psoriasis and inflammatory changes in joints. The anatomical connection between the nail matrix and the enthesis of the distal interphalangeal joint extensor was proved. The whole structure is called a joint-entheseal-nail apparatus . As the DIP joints are the most often affected in PsA, involvement of this complex can be a possible explanation of considerably higher concomitance of nail changes in those patients. It was confirmed in the studies by imaging early or advanced inflammation in DIP joints and entheses by ultrasound and high-resolution MRI . The entheses, like the skin, are exposed to both shear and compressive forces, which causes lesion spreading according to the Koebner phenomenon mechanical stress and microdamage in DIP joints can result in psoriatic nails.
Some reports indicate that nail psoriasis is associated with a few predisposing factors. It was proven that nail changes are more frequently observed in patients with a long history of psoriasis vulgaris, early onset of psoriasis, higher score of Psoriasis Area and Severity Index and with concomitant PsA .
Nail Psoriasis Is A Notable Characteristic In Many But Not All Patients With Psoriatic Arthritis This Study Is An Attempt To Obtain More Specific Detailed Information About The Connection Between These Conditions As Well As Their Implications
The vast majority of patients with psoriatic arthritis have nail changes and these nail changes are likely due to active enthesitis of the distal extensor tendon, Shari Lipner MD, PhD, told MedPage Today. In addition, many patients with nail psoriasis have underlying psoriatic arthritis, commented Dr. Lipner, whos Associate Professor of Clinical Dermatology and Director, Nail Division, at Weill Cornell Medicine in New York, NY.
Take Note
- “Nail psoriasis should be treated early with therapy dictated by the number of nails involved, severity of disease, involvement of skin and joints, co-morbidities, and impact on quality of life…Theres an unmet need for development of clinical trials that specifically address nail psoriasis, rather than a subset analysis of cutaneous psoriasis patients.” Shari Lipner, MD, PhD
Why its a big deal
Theres a strong association between nail psoriasis and the development of psoriatic arthritis , with 3 times as many people with nail disease developing PsA compared with those who dont have any signs of nail changes. Nail psoriasis has been linked through imaging studies to enthesitis, which manifests in early stages of PsA. 1
What we dont know
Our results show that nail psoriasis was associated with an overall higher burden of disease in all domains of PsA, the study authors reported.
Real-world U.S. data analyzed
Burden of nail disease imposed by PsA
PsA, with and without nail involvement
Clear clinical implications
Recommended Reading: Can Nail Fungus Be Cured
Clinical Trials Evaluating Efficacy In Np
The 1546 articles identified by the literature search for approved systemic drugs included 66 clinical studies that reported outcomes for NP. Nail measures were a primary study outcome in 22 of the included articles, a secondary outcome in 25 articles, and a retrospective or posthoc outcome in the remaining 19. Half of the articles reported data for various patient subgroups, including one with nail symptoms at baseline, and half were analyses that reported data only for patients with nail symptoms. Nineteen articles reported prospective studies dedicated to NP , and the remainder were subgroup analyses . Moderate or severe PsO ± PsA was a clinical trial inclusion criterion in 33 articles, active PsA an inclusion criterion in 9 articles, and PsO and/or PsA in 6.
Twenty-two of the included articles reported placebo-controlled trials, including 5 articles reporting trials that also included an active comparator , and 5 articles reported head-to-head trials with no placebo arm. Sixty-one articles reported trials focused on single agents, including nonbiologics TNF, IL-12/23, IL-17A, and IL-23 inhibitors and targeted synthetic disease-modifying antirheumatic drugs.
Nail Assessment And Scoring Systems

Overall clinical severity has been described using the fingernail physician global assessment ,,, by which the fingernails are assessed for nail plate pitting, crumbling, onycholysis, oil-drop discoloration, and/or nail bed hyperkeratosis on a 5-point scale, from 0 to 4 , and by simple visual analog scale . The need for more precise outcome measures to determine therapeutic efficacy in clinical trials has led to several more complex scoring systems .
Comparison of nail scoring systems used in studies of currently approved treatments for PsO and/or PsA.
The Nail PsO Area Severity Index is the most widely used tool for scoring NP in clinical trials. Using the NAPSI, each nail is divided into 4 quadrants and scored based on the presence or absence of psoriatic changes to the nail matrix and the nail bed ., The NAPSI usually assesses fingernails, for a total score of 080, but some studies have also included the toenails . The NAPSI is the only system that explicitly separates nail matrix and nail bed symptoms.
Overview of dedicated, prospective NP studies of currently approved treatments for PsO and/or PsA.
Five other nail scoring systems are used less frequently: Psoriasis Nail Severity Score,, Baran system, Cannavò system, Nail Area Severity score, and NijmegenNail PsO Activity Index tool , which combines the elements from other systems that best predicted clinical assessments .
Also Check: What Vitamin Is Good For Hair And Nails
Wear Gloves When Working With Your Hands
This includes housework, yard work, and home repairs. Any time you irritate your skin or nails, psoriasis can flare. When doing wet work like washing dishes, its best to wear a cotton glove and then place a vinyl or nitrile glove over it. According to the American Academy of Dermatology, latex gloves dont give your nails enough protection. Keeping nails dry can also make infections less likely.
Splitting With Purple Spots
Splitting of the nail may be related to nail ridges. It is possible that the purple spots are the result of splinter hemorrhages that occur in the grove or ridge that has formed on the nail. However, it is important to note that if you are seeing a dark streak, often on the thumb or big toe of your dominant hand or foot, this could also be a sign of nail-melanoma and it is important to get a quick consult from your dermatologist.
You May Like: How To Quit Biting Nails
Ra Vs Psoriatic Arthritis Nail Changes
RA and PsA are both autoimmune conditions that cause joint pain and nail changes. So whats the diff?
PsA is a mixture of psoriasis and arthritis symptoms that often hits that last finger joint the hardest. Not everyone with RA has nail-related symptoms, but folks with PsA are much more likely to have skin and nail symptoms. In fact, about 80 percent of people with PsA experience nail changes.
People with PsA are also more likely to experience nail pitting and more painful nail splitting that can lead to infections. Ridges and nail separation can also occur.
To treat RA nail changes, you have to treat the disease first. Doctors may prescribe medications such as disease-modifying antirheumatic drugs and biological response modifiers to help treat RA symptoms.
Your doc may recommend other lifestyle changes to help reduce and manage RA symptoms, such as:
- Exercising. You could try walking, swimming, or biking for 30 minutes per day, 5 days per week.
- Taking movement classes for arthritis. Some gyms and community centers have classes focused on the mobility and pain management needs of people with joint problems.
- Trying to quit smoking. A history of smoking may increase your risk of developing RA, and continued smoking may make symptoms worse.
- Getting enough rest. Give yourself a break. Too much stress may contribute to symptoms.
- Changing your diet. Eating more foods that reduce inflammation may help your symptoms.
When To See A Doctor
If you notice anything suspicious going on with your nails, its probably time to chat with a healthcare pro, because nail psoriasis could be an early symptom of PsA. Either way, you may need treatment if something like a fungal infection has developed.
Likewise, if youre living with PsA and you develop new nail symptoms, its time for a checkup. You may need to change up your treatment dose or ask about other options.
Keep in mind that your nails grow slowly, so any medications youre using may take time to show their positive effects. Be a patient patient and remember to keep your doc updated with any changes.
Finding the right treatment to ease your symptoms may involve a hefty dose of trial and error. But working with your doctor gives you the best chance of getting the results you want.
Also Check: Where Can I Buy Nail Polish Strips
How Are Psoriatic Arthritis Nail Problems Treated
There are many treatments your dermatologist may recommend for your nails if they are impacted by psoriatic disease. Some of the treatments are applied directly on the nails. These include medications such as corticosteroids, calcipotriol , and tazarotene , according to the American Academy of Dermatology. Your derm may also recommend laser treatment on the affected nail or UVA ray exposure. There are also medicines that work inside your body that can , including: biologics, methotrexate, retinoid, cyclosporine, and apremilast.
While these are proven treatments, it may still require some patience when it comes to healing according to Dr. Sayed. Nail damage can improve with treatment but can be frustrating because it takes longer to improve than skin, he says. Skin replaces itself about every four weeks so you can see dramatic improvement with treatment within that time. Fingernails take about six months to grow out so it takes at least that long for normal nails to replace the old, damaged nails. And toenails can really test your patience, sometimes taking over a year to improve. Just like the skin, everyone responds differently to treatments and sometimes you have to try a few to find the best response, Dr. Sayed explains.
Guidelines For Treatment Of Np
In 2015, the Group for Research and Assessment of PsO and PsA included NP as one of the 6 key domains of PsA . For treatment of patients with moderate-to-severe NP, the 2015 GRAPPA treatment guidelines recommended biologic treatment with TNF, IL-12/23, and IL-17 inhibitors, choosing therapy to address as many disease domains as possible.
The recently published Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with biologics recommended biologic monotherapies for treatment of adult patients with moderate to severe plaque PsO affecting the nails .
You May Like: Where To Buy Breathable Nail Polish
Help For Hands And Fingers
Medicines you take for PsA can control inflammation and ease swelling and aches in your hands and fingers. The type of treatment you need depends on your symptoms and how severe they are. For example, sausage digits often happen in people who have severe PsA, so your doctor may recommend a strong medicine like a biologic.
You can also do a lot on your own to get relief.
- Try cold packs. To bring down swelling, wrap a bag of frozen veggies or ice cubes in a soft towel. Place it on your hand for 10 minutes on, then 10 minutes off. You can do it for up to an hour.
- Take work breaks. When youâre writing or typing, give your hands a rest every 30 minutes or so.
- See a physical or occupational therapist. They can show you new ways to do things that donât hurt your hands.
- Go for gadgets. Some tools are made especially for sore hands, like easy-grip pens and nonslip jar openers. Your doctor or physical therapist can tell you where to find them.
- Do hand exercises. These keep your hands and fingers strong and flexible. You can find examples online or ask your physical therapist to show you some.
Nail Symptoms With Psoriatic Arthritis
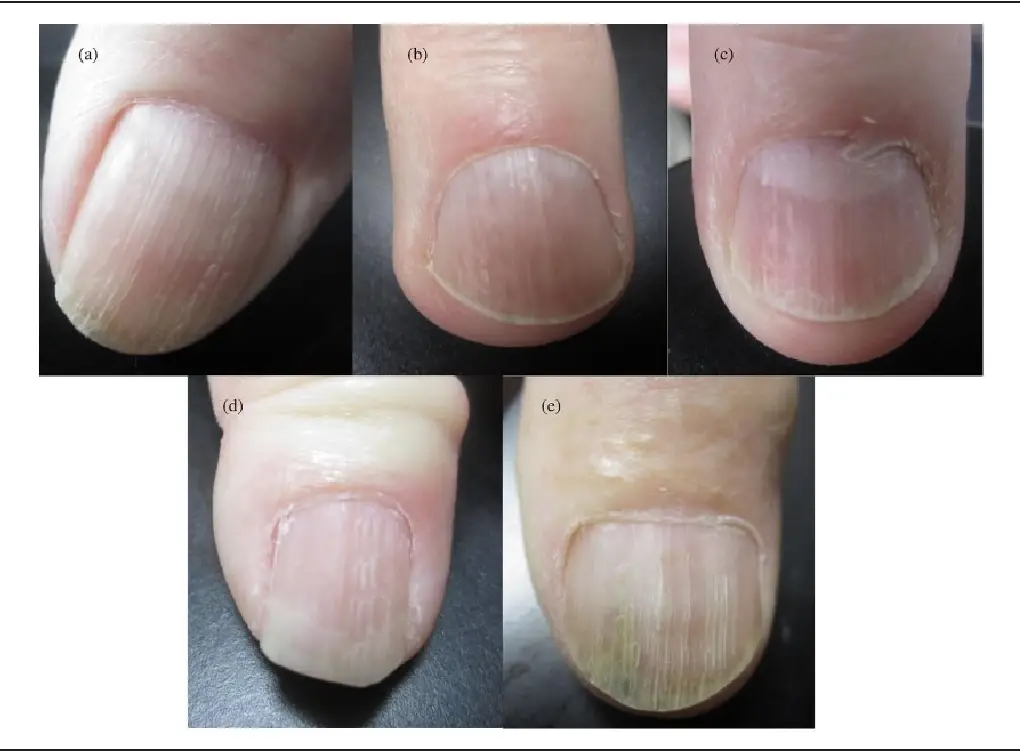
Psoriasis can affect any of the structures of the nail matrix and nail bed, depending on the duration and location of psoriasis within the nail formation. Nail psoriasis is characterized by a number of symptoms, such as:
- Pitting, or small depressions on the nail
- Crumbling, which represents a merging of pitting due to a longer duration of nail psoriasis
- Psoriatic leukonychia, appearing as white spots in the nail
- Red dots in the crescent shape at the base of the nail
- Oil drop or salmon patch discoloration, named because it resembles a drop of oil or is reddish like a salmon
- Nail bed hyperkeratosis, an abnormal thickened layer of skin beneath the nail
- Splinter hemorrhages, small areas of bleeding that run in the direction of nail growth
- Onycholysis, lifting of the nail or separation from the nail bed1,3
- Pain
- Inability to grasp small objects, tie shoe laces or button clothes
- Altered sense of fine touch
Nail psoriasis is highly visible and can have a substantial impact on the person’s quality of life and psychological health.
Also Check: How Do You Remove Sally Hansen Gel Nail Polish
Treatment Of Nail Psoriasis
Treatment of nail psoriasis is a clinical challenge. The methods of treatment should be adjusted to the extent of skin diseases, psoriatic arthritis, severity of nail changes and impairment of the quality of life. Topical products, procedural intervention, and systemic and biological agents are possible options for treatment. There are many impediments to therapy including poor penetration of topical products, adverse effects of systemic and biologic treatment, monitoring of improvements and patients attitude .
Topical products are highly recommended in cases of patients with psoriasis limited to the nails, with minimal or without skin disease, and with no evidence of arthritis. Strong topical corticosteroids alone or in combination with calcipotriol are the best therapeutic option in these cases . Intralesional injection of corticosteroids may be effective therapy but implies adverse effects such as pain of injection, skin atrophy, depigmentation, secondary infection and subungual haemorrhage. Triamcinolone acetonide 0.10.2 ml of 510 mg/ml is most frequently used in injection. Nerve blockers or topical anaesthetics are necessary during procedures to reduce the pain .
Biological therapy is a great achievement in nail psoriasis treatment. The recommendations for therapy, in ranked order from the highest to lowest, are adalimumab, etanercept, ustekinumab, infliximab, apremilast and golimumab .
How To Treat And Care For Psoriatic Arthritis Nails
Its best to err on the side of caution and consult with your physician if youre at all worried about your nails, Dr. Garshick says. For any individual who has psoriatic arthritis and is experiencing any nail changes, it is always a good idea to talk with your doctor, since it can be important to determine if it is related to psoriasis or not, Dr. Garschick says.
Dr. Paviol suggests tracking your nail changes and how long theyve been happening in a journal. It can be helpful to make notes of other psoriatic arthritisrelated changes, such as new joint symptoms and any skin lesions. If you experience any of these nail changes and joint pain , then you may want to talk to your dermatologist or rheumatologist if you have one.
In terms of treatment, your doctor may prescribe a pharmacological medication that targets just your nail symptoms or a medication that treats your psoriatic arthritis overall. Ultimately, the treatment will depend on your specific situation.
Importantly, while some of these medications have been studied specifically for the treatment of nail psoriasis, if someone is struggling with nail psoriasis and psoriatic arthritis, it is important to consider both of these factors when selecting a treatment to be sure to select a medication that will work well for both, explains Dr. Garshick.
Related:
Read Also: How To Prevent Nail Biting
Nail Psoriasis An Early Sign Of Psoriatic Arthritis
Nail psoriasis can be an early sign of psoriatic arthritis. Previous research has found that at least 80 percent of people with psoriatic arthritis may also have nail psoriasis. A Canadian study looked at 188 people with psoriatic arthritis to determine if these changes to the nails were associated with specific joint symptoms. Of the group, 172 patients had some form of fingernail psoriasis on at least one nail.
Patients with blood spots under the nails known as splinter hemorrhages were found to have a higher number of swollen joints, compared to those with other nail psoriasis symptoms. The type of symptoms a patient had gave insight into what was happening with the joints. Researchers found that those patients with nail crumbling, separation of the nail from the skin under the nail, and a buildup of keratin under the nail were more likely to have a swollen or tender distal interphalangeal joint on the same finger. DIP joint is the finger joint closest to the nail.
The researchers suggest that patients with psoriatic arthritis should have their fingernails examined.
Severity Of Nail Disease And Skin Disease
Severe nail disease as measured by the PNSS was strongly associated with severe skin disease . The PNSS correlated with percentage body surface area affected by psoriasis and physician global assessment of psoriasis . In addition, other indicators of skin severity such as the number of psoriasis treatments and hospital admissions for psoriasis were associated with severe nail disease. However, there was no association with particular patterns of skin disease and the severity of nail disease.
Severe nail disease measured by the PNSS is associated with severe psoriasis as indicated by %BSA affected by psoriasis, physician global assessment of psoriasis, number of treatments for psoriasis and hospital admissions for psoriasis. Error bars indicate SEM.
Also Check: What Do You Need To Do Gel Nails
